Tibial plateau fractures are commonly due to high-energy trauma, though they may occur following low-energy trauma in elderly osteoporotic patients.
They may be associated with neurovascular, ligamentous, and/or meniscal injury.
Features of the Medial Plateau:
✯ Concave
✯ Slightly inferior
✯ Bears 60% of the weight
✯ Stronger than the lateral plateau
Features of the Lateral Plateau:
✯ Convex
✯ Extends more superior
✯ More commonly fractured
Commonality of fracture:
Lateral > Bicondylar > Medial
Soft tissue and ligamentous injuries are common in tibial plateau fx. A careful physical exam is important to assess for:
✯ Compartment Syndrome
✯ Neurovascular injury
✯ Ligamentous Injury
✯ Open Fracture
Assessing knee ligaments will most likely be difficult due to pain.
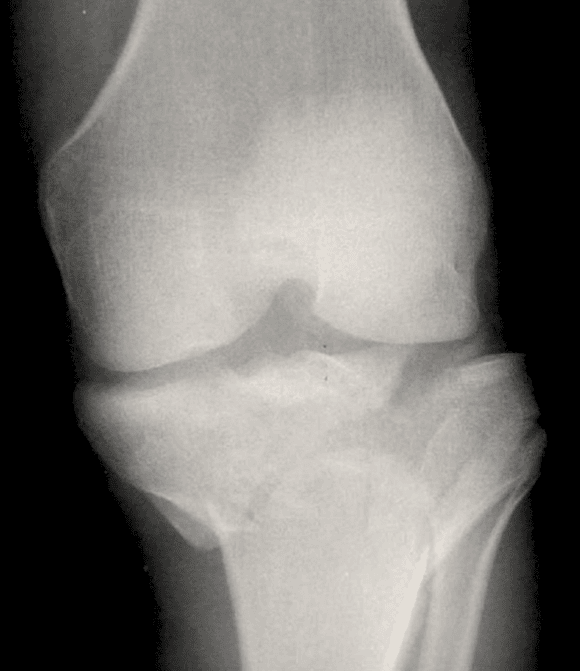
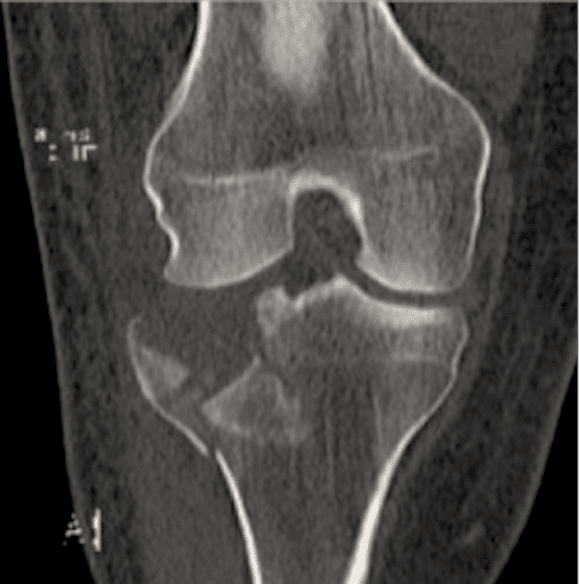
In addition to knee radiographs, a CT scan should also be obtained.
A 1997 study by Chan et al showed that surgical planning was changed in 26% of cases after viewing CT scan vs. plain radiographs.
Traction views may reduce bony overlap in severely impacted/comminuted fractures
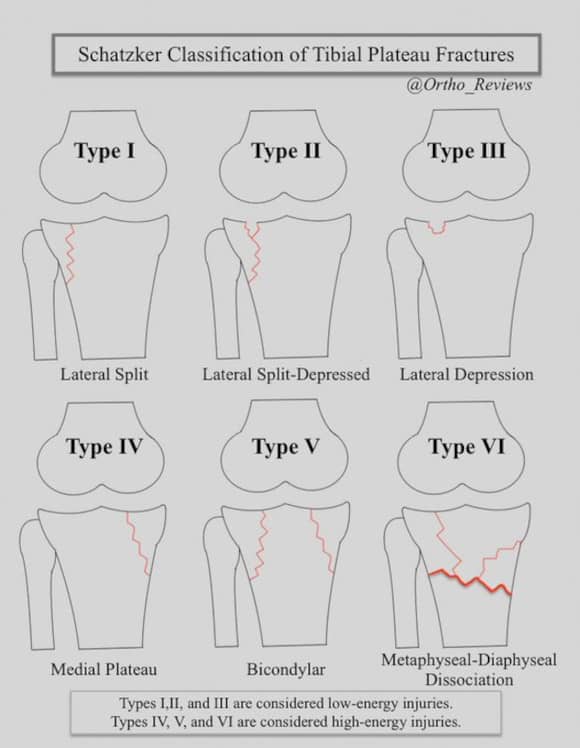
The Schatzker classification system is commonly used for tibial plateau fractures:
✯Type I: lateral split
✯Type II: lateral split-depression
✯Type III: isolated lateral depression
✯Type IV: medial split
✯Type V: bicondylar
✯Type IV: metaphyseal-diaphyseal dissociation
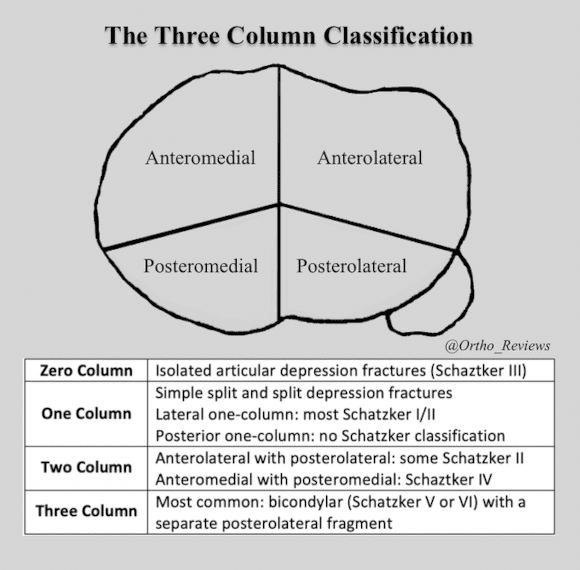
Tibial plateau fractures may also be classified using a three-column system based on transverse CT imaging.
Fractures may be zero, one, two, or three-column.
It has been proposed that some Shatzker type IV, medial plateau fractures, are the result of knee dislocations that have spontaneously reduced.
These injuries are associated with a higher risk of neurovascular injury.
Meniscal injury has been reported to occur in up to 50% of tibial plateau fractures.
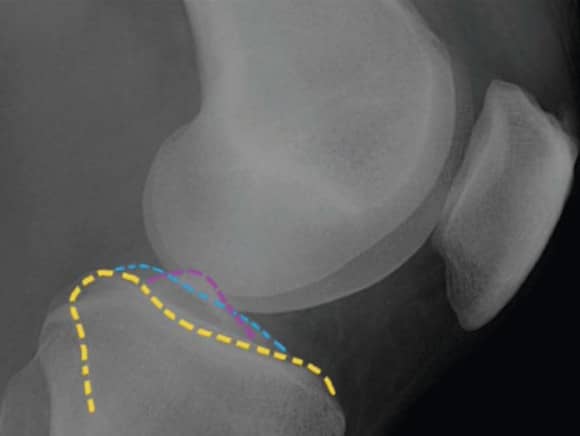
It's been suggested that there's an increased risk of meniscal injury in lateral plateau fractures with:
✯ >6 mm articular depression
✯ >5 mm articular widening
Non-operative management may be an option for minimally displaced fractures and small depression fractures. As well as for non-ambulatory patients and poor surgical candidates
Non-operative treatment:
Protected weight-bearing utilizing a hinged knee brace with early passive ROM
Operative Indications:
✯ > 1 cm metaphyseal-diaphyseal translation
✯ > 2mm intra-articular step-off
✯ > 10° angular deformity
✯ Schatzker types IV, V, and VI
✯ Open Fracture
✯ Vascular Injury
The most important objective is restoration of the articular surface.
Temporary external fixation is commonly utilized in patients with extensive soft tissue injury and polytrauma patients. It has been shown to reduce infection and wound complication rates.
Definitive management is commonly performed 7-14 days later.

A 2009 @jbjs study by Hall et al showed that definitive treatment with circular external fixation and minimal internal fixation may be an effective treatment option with similar outcomes to ORIF for bicondylar fractures, with a ↓ hospital stay: 9.9days vs 23.4 days, respectively
Treatment of Schatzker types I-IV may potentially be treated with closed reduction and percutaneous screw fixation if reduction can be maintained with < 1 mm articular step-off.
If unable to maintain reduction, ORIF with unilateral plating may be performed.
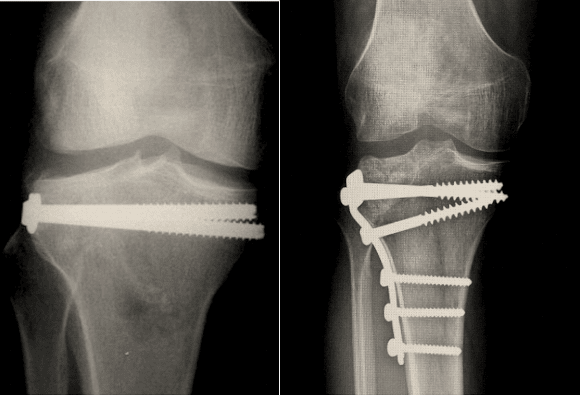
Bicondylar fractures, Schatzker Type V and VI, may be treated by dual plating (shown below) or with definitive external fixation with minimal internal fixation.

A 2014 @jbjs study by Wasserstein et al, showed that at 10-year follow-up, 7.3% of patients who had undergone surgical management of tibial plateau fractures had a knee replacement performed.
Which was 5 times more likely than the general population control group.
It has been suggested that in some instances acute total knee replacement may be an acceptable option for the treatment of tibial plateau fractures in patients > 65 y.o., those with pre-existing osteoarthritis and/or osteoporosis.
Complications:
✯ Post-traumatic arthritis
✯ Hardware failure
✯ Malunion: most common in Schatzker type VI
✯ Infection: these injuries are at an increased risk of infection due to extensive soft tissue injury
References:
1: https://pubmed.ncbi.nlm.nih.gov/28461952/
2: https://pubmed.ncbi.nlm.nih.gov/25820894/
3: https://pubmed.ncbi.nlm.nih.gov/21763651/
4: https://pubmed.ncbi.nlm.nih.gov/29145966/
5: https://pubmed.ncbi.nlm.nih.gov/28461952/
6: https://pubmed.ncbi.nlm.nih.gov/20881634/